What is it?
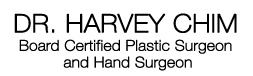
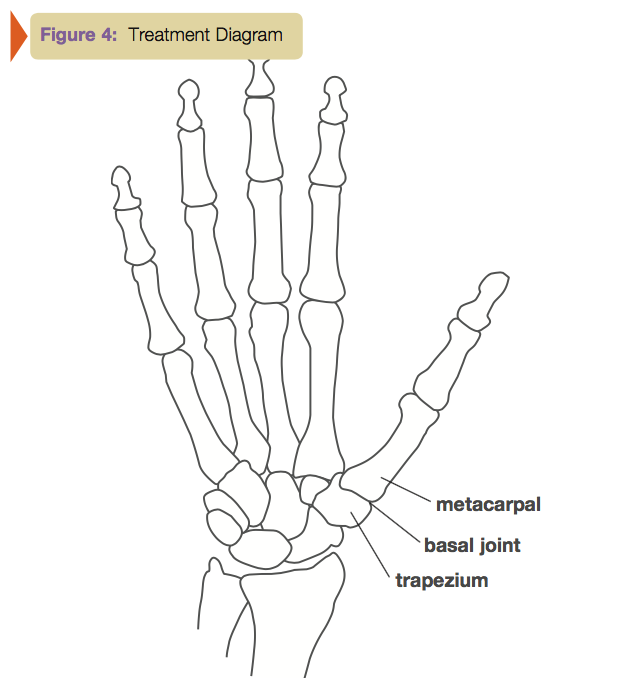
In a normal joint, cartilage covers the end of the bones and serves as a shock absorber to allow smooth, pain-free movement. In osteoarthritis (OA, or “degenerative arthritis”) the cartilage layer wears out, resulting in direct contact between the bones and producing pain and deformity. One of the most common joints to develop OA in the hand is the base of the thumb. The thumb basal joint, also called the carpometacarpal (CMC) joint, is a specialized saddle-shaped joint that is formed by a small bone of the wrist (trapezium) and the first bone of the thumb (metacarpal). The saddle shaped joint allows the thumb to have a wide range of motions, including up, down, across the palm, and the ability to pinch (see Figure 1).
Who gets it?
OA at the base of the thumb is more commonly seen in women over the age of 40. The exact cause is unknown, but genetics, previous injuries such as fractures or dislocations, and generalized joint laxity may predispose towards development of this type of arthritis.
What are the symptoms and signs?
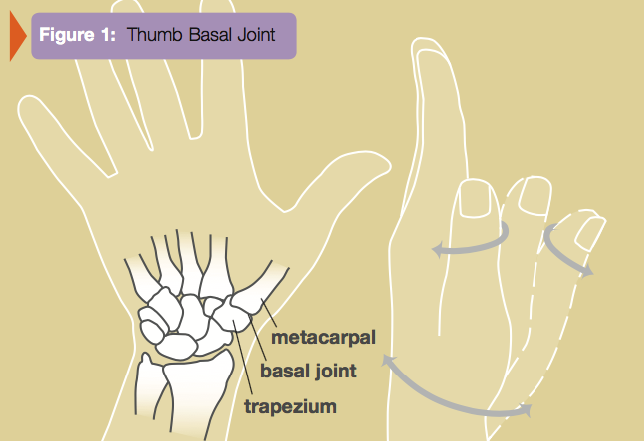
The most common symptom is pain at the base of the thumb. The pain can be aggravated by activities that require pinching, such as opening jars, turning door knobs or keys, and writing. Severity can also progress to pain at rest and pain at night. In more severe cases, progressive destruction and mal-alignment of the joint occurs, and a bump develops at the base of the thumb as the metacarpal moves out of the saddle joint. This shift in the joint can cause limited motion and weakness, making pinch difficult (see Figure 2). The next joint above the CMC may compensate by loosening, causing it to bend further back (hyperextension).
How is the diagnosis made?
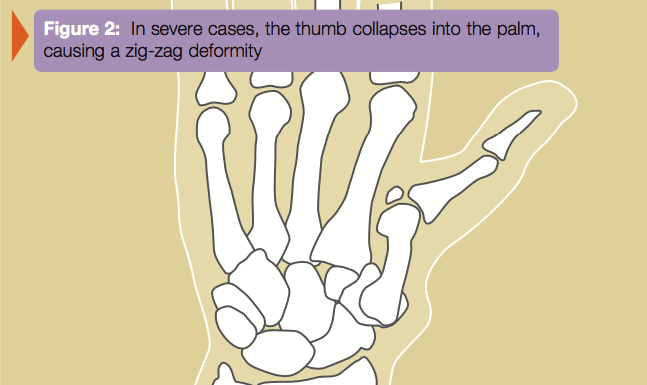
The diagnosis is made by history and physical evaluation. Pressure and movement such as twisting will produce pain at the joint. A grinding sensation may also be present at the joint (see Figure 3). X-rays are used to confirm the diagnosis, although symptom severity often does not correlate with x-ray findings.
What are the treatment options?
Less severe thumb arthritis will usually respond to non-surgical care. Arthritis medication, splinting and limited cortisone injections may help alleviate pain. A hand therapist might provide a variety of rigid and non-rigid splints which can be used while sleeping or during activities.
Patients with advanced disease or who fail non-surgical treatment may be candidates for surgical reconstruction. A variety of surgical techniques are available that can successfully reduce or eliminate pain. Surgical procedures include removal of arthritic bone and joint reconstruction (arthroplasty), joint fusion, bone realignment, and even arthroscopy in select cases. A consultation with your hand surgeon can help decide the best option for you (see Figure 4).
Dr Chim offers two procedures. The first is trapeziectomy with tendon interposition, which is the gold standard for basal joint arthritis. The second involves joint replacement- Dr Chim uses the Stablyx implant, which allows for a very stable joint and increased pinch strength. The surgery is done in an ambulatory surgery center and patients can go home the same day.
Adapted from educational material from the ASSH (American Society for Surgery of the Hand).